Posner-Schlossman syndrome, also known as glaucomatocyclitic crisis, is characterized by distinct symptoms and signs. Here’s a breakdown of the typical manifestations associated with this condition:
case report
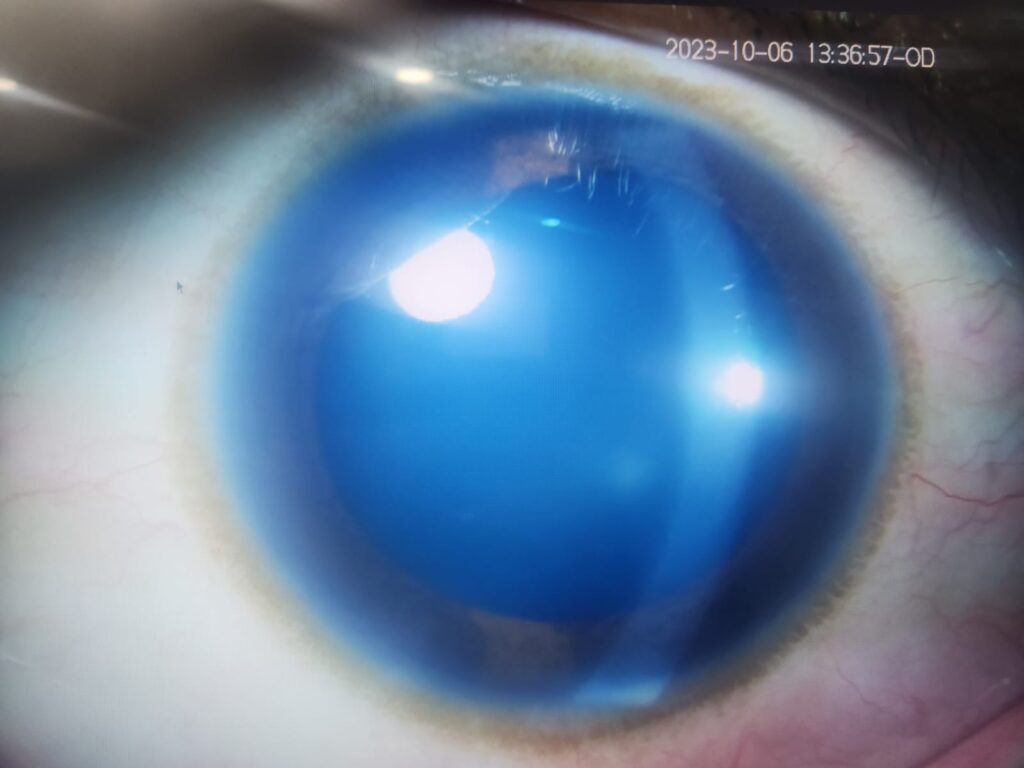
A 16 year old female presented to our opd with chief complaint of right eye decrease of vision and redness of eyes for 1 day. Her vision was noted to be right eye-6/6 p and left eye 6/6 . There was slight conjuctival redness in right eye. cornea of right eye was slightly hazy compared to left eye. on gonioscopy angles of both eyes were open. Intra ocular pressure od -56 mm of hg and le 23 mmhg . Posterior segment examination was normal. Disc was normal with 0.3 cupping in both eyes. Based on above clinical findings the diagnosis of right eye Posner-Schlossman syndrome was made and treatment was done accordingly.

Symptoms:
- Sudden Onset of Eye Pain: Individuals with Posner-Schlossman syndrome often experience a sudden, sharp pain in the affected eye. This pain may range from mild discomfort to more severe and debilitating sensations.
- Redness of the Eye (Conjunctival Injection): The white part of the eye, known as the conjunctiva, becomes visibly red and inflamed. This redness is a common and noticeable symptom.
- Blurred Vision: Vision in the affected eye may become blurry or hazy during an episode. This can significantly impact visual acuity.
- Halos Around Lights: Some individuals may perceive halos around lights, particularly in low-light environments. This can be a result of elevated intraocular pressure.
- Photophobia (Light Sensitivity): Sensitivity to light, or photophobia, may be experienced. Bright lights can exacerbate discomfort.
Signs:
- Elevated Intraocular Pressure (IOP): One of the primary signs of Posner-Schlossman syndrome is an increase in the pressure inside the eye. The IOP is often markedly elevated, usually 40-50 mmHg. Characteristically, IOP elevation is out of proportion to the amount of anterior chamber inflammation, and significant corneal epithelial edema may develop. This elevation in IOP is often a transient feature and may last from several hours to weeks and may precede or follow the anterior chamber reaction during acute episodes.
- Mild Anterior Chamber Inflammation: While not a prominent feature, there may be some degree of inflammation in the anterior chamber of the eye. This differs from other forms of uveitis where inflammation is typically more pronounced.
- Clear Cornea: Unlike many other forms of glaucoma, the cornea (the clear front surface of the eye) remains clear in Posner-Schlossman syndrome.
- Normal Angle Structures: The angle structures, particularly the trabecular meshwork responsible for draining aqueous humor, appear normal on examination.
- No Ocular Damage Between Episodes: In between episodes, there is typically no evidence of optic nerve damage or visual field loss, which distinguishes Posner-Schlossman syndrome from other forms of glaucoma.The optic nerve can demonstrate acute glaucomatous cupping during an acute attack, as well as decreased perfusion due to the sharp rise in IOP. However, many patients present with normal appearing nerves in an active episode. Cupping may reverse after the IOP returns to normal. In cases of repeated attacks over a long period of time, persistent glaucomatous cupping may be observed indicating some degree of permanent damage to the optic nerve.
Management:
- Diagnosis:
- Diagnosis of Posner-Schlossman syndrome is based on a thorough clinical evaluation by an ophthalmologist.
- Detailed medical history, including any previous episodes, is important for accurate diagnosis.
- Differentiating features such as the absence of significant inflammation and clear cornea are key indicators.
- Diagnostic Tests:
- Tonometry: Measures intraocular pressure (IOP). Elevated IOP during an episode is a hallmark of this syndrome.
- Slit Lamp Examination: Allows detailed examination of the anterior segment of the eye, including the cornea, iris, and anterior chamber. Signs of inflammation may be observed.
- Gonioscopy: Evaluates the angle between the iris and cornea, checking for any blockages in the trabecular meshwork.
- Visual Field Testing: Helps assess any potential vision loss or abnormalities.
- Optical Coherence Tomography (OCT): Provides high-resolution images of the retina, aiding in the evaluation of optic nerve health.
- Treatment:
- Topical Medications:
- Anti-glaucoma Medications: Eye drops like beta-blockers, prostaglandin analogs, and carbonic anhydrase inhibitors are used to lower intraocular pressure.
- Steroids: Topical steroids may be prescribed to manage any mild inflammation present.
- Oral Medications:
- In some cases, oral medications like acetazolamide may be prescribed to further lower intraocular pressure.
- Follow-up and Monitoring:
- Regular follow-up appointments with an ophthalmologist are crucial to monitor IOP, visual function, and any potential changes.
- Surgery (in Severe Cases):
- While rare, if medical treatment is insufficient, surgical options like trabeculectomy or glaucoma drainage devices may be considered.
- Management of Recurrent Episodes:
- During acute episodes, additional topical medications and close monitoring may be required.
- Patient Education:
- Educating the patient about the condition, its episodic nature, and the importance of timely treatment and follow-up is essential.
- Topical Medications:
- Lifestyle Considerations:
- Stress reduction techniques and maintaining a healthy lifestyle may help in managing the condition.
- Education and Support:
- Patients benefit from understanding their condition and its management. Support groups or patient resources may be helpful.
It’s important to note that individual cases may vary, and treatment approaches should be tailored to each patient’s specific needs. Early diagnosis and consistent follow-up care are crucial in effectively managing Posner-Schlossman syndrome and preserving vision.

