Diabetic retinopathy is a serious complication of diabetes that affects the eyes. It occurs when high blood sugar levels damage the blood vessels in the retina, the light-sensitive tissue at the back of the eye. There are two main stages of diabetic retinopathy: non-proliferative and proliferative.
Non-proliferative diabetic retinopathy (NPDR) is an early stage of diabetic retinopathy. In this stage, the small blood vessels in the retina are weakened and may leak fluid or blood. This can lead to swelling or the formation of deposits in the retina.
There are different levels of NPDR, ranging from mild to severe. In the mild stage, there may be small areas of swelling or microaneurysms, which are tiny bulges in the blood vessels. As NPDR progresses, more blood vessels become affected, and the condition can become moderate or severe.
Diabetic macular edema (DME) is a complication of diabetic retinopathy, involves swelling in the macula, which is the central part of the retina responsible for sharp, central vision.
The macula is essential for tasks that require detailed vision, such as reading, recognizing faces, and driving. When it becomes swollen from fluid leakage, it can lead to significant visual impairment.

Proliferative diabetic retinopathy (PDR) is an advanced stage of diabetic retinopathy, a serious complication of diabetes. In PDR, abnormal blood vessels begin to grow on the surface of the retina. These new vessels are fragile and can bleed easily, leading to further complications and potential vision loss.
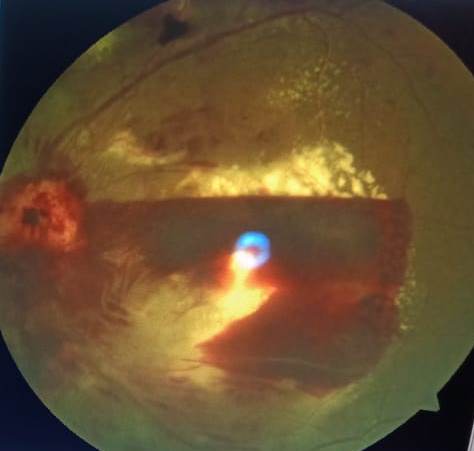
The growth of these abnormal vessels is a response to the reduced blood flow caused by the damaged vessels in the earlier stages of diabetic retinopathy. The body attempts to compensate by creating new vessels, but these are often weak and prone to bleeding(Vitreous hemorrhage). Moreover, scar tissue may form, which can lead to retinal detachment (Tractional retinal detachment ) if not treated promptly.
Investigations
The investigation for diabetic retinopathy typically involves a combination of clinical examinations and specialized tests to assess the condition of the retina and the severity of retinopathy. Some common investigations for diabetic retinopathy:
- Dilated Fundus Examination: This is a standard procedure where the ophthalmologist uses eye drops to dilate the pupils, allowing them to examine the inside of the eye, including the retina and optic nerve.
- Visual Acuity Test: This test measures how well you can see at various distances using an eye chart. It helps determine the clarity of your vision.
- Tonometry: This test measures the pressure inside your eyes. Elevated pressure can be a sign of glaucoma, a condition that can occur alongside diabetic retinopathy.
- Fluorescein Angiography: A special dye (fluorescein) is injected into a vein in your arm. The dye travels through the blood vessels in the retina, highlighting any abnormalities or leakage. Photographs are taken to document the blood flow.
- Optical Coherence Tomography (OCT): This is a non-invasive imaging test that uses light waves to take cross-sectional pictures of your retina. It provides detailed information about the layers of the retina and helps in assessing the presence of fluid or swelling.
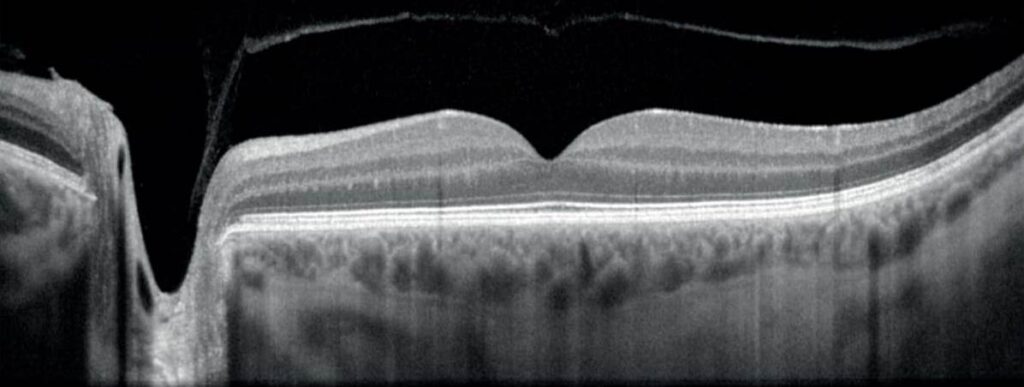
OCT is a powerful tool for monitoring the progression of diabetic retinopathy and assessing the effectiveness of treatments. Regular OCT scans are often recommended for individuals with diabetes, especially those at risk for or diagnosed with diabetic macular edema. It allows for early detection and intervention, which is crucial in preserving vision and preventing further damage. OCT can pick following finding in retina in a case of diabetic macular edema:
Macular Edema: OCT is particularly effective in identifying and quantifying diabetic macular edema (DME). It shows areas of fluid accumulation in the macula, which is the central part of the retina responsible for detailed vision.

Retinal Thickening: OCT measures the thickness of the retinal layers. In DR, areas of retinal thickening can be indicative of fluid accumulation due to leaking blood vessels.
Intraretinal Cysts: These are fluid-filled spaces within the layers of the retina. They appear as dark areas on the OCT scans and are a common finding in cases of DME.
Epiretinal Membrane (ERM): OCT can identify the presence of a thin, fibrous membrane on the surface of the retina. This can occur in advanced stages of DR and may contribute to visual distortion.

Vitreoretinal Interface Abnormalities: OCT can detect any abnormalities in the interface between the vitreous (the gel-like substance inside the eye) and the retina. This is important in cases where there is traction on the retina, which can lead to retinal detachment.
Subretinal Fluid: In advanced cases of DR, fluid can accumulate between the layers of the retina, a condition known as serous detachment.
Hyper-reflective Lesions: OCT can reveal hyper-reflective spots or lesions within the retinal layers. These can be indicative of microaneurysms or areas of hemorrhage.
Loss of Retinal Layers: In severe cases of DR, there may be disruption or loss of certain retinal layers, particularly in the outer segments.
Neovascularization: OCT angiography, a specialized variant of OCT, can be used to visualize the growth of abnormal blood vessels (neovascularization) in more detail.
- Ultrasound of the Eye: In some cases, especially if there is bleeding inside the eye, ultrasound may be used to get images of the eye’s interior.
- Retinal Photography: High-resolution images of the retina may be taken to document any changes over time.
- Gonioscopy: This is a test used to examine the drainage angle of the eye, which is important in conditions like neovascular glaucoma that can occur due to advanced diabetic retinopathy.
- Electroretinography (ERG): This test measures the electrical activity in the retina, helping to assess the health of the cells that detect light.
- Blood Pressure Measurement: Monitoring blood pressure is important, as uncontrolled high blood pressure can exacerbate diabetic retinopathy.
Symptoms
While NPDR may not initially cause noticeable symptoms, it’s crucial to monitor it closely. Regular eye exams are essential for individuals with diabetes to detect any changes in the retina early on. Good blood sugar control and managing other aspects of diabetes, such as blood pressure and cholesterol levels, can also help slow the progression of NPDR.
Symptoms of DME can include blurred or distorted central vision, difficulty reading, and a sense of haziness or darkness in the center of the visual field. It’s worth noting that these symptoms may develop gradually and may not be immediately noticeable.
Symptoms of PDR may include a sudden increase in floaters (small, dark spots or lines in your field of vision), blurred or cloudy vision, and even sudden vision loss. However, it’s possible for PDR to develop without noticeable symptoms, underlining the importance of regular eye exams for individuals with diabetes.
Treatment
Systemic factor control plays a crucial role in the management of diabetic retinopathy (DR), as it directly impacts the progression and severity of the condition. Here are the key systemic factors and their role in DR:
- Blood Glucose Control: Maintaining optimal blood glucose levels is paramount in preventing and managing DR. Elevated blood sugar levels over time can damage the blood vessels in the retina, leading to the development and progression of DR. Tight glycemic control through diet, exercise, and medication (if prescribed) is essential.
- Blood Pressure Management: High blood pressure (hypertension) is a significant risk factor for DR. Elevated blood pressure can further damage the already compromised blood vessels in the retina. Controlling blood pressure through lifestyle modifications and, if necessary, medication, can help slow the progression of DR.
- Cholesterol Levels: Elevated levels of LDL cholesterol can contribute to the development and progression of DR. Managing cholesterol levels through diet, exercise, and medication (if prescribed) can help mitigate this risk.
- Kidney Function: Diabetes can lead to kidney disease (nephropathy), which is closely linked to DR. Monitoring kidney function and managing any kidney-related issues can indirectly benefit the eyes.
- Smoking Cessation: Smoking is a significant risk factor for DR and can exacerbate existing retinal damage. Quitting smoking can help reduce the risk of further complications.
- Regular Medical Check-ups: Regular visits to a healthcare provider for diabetes management and overall health monitoring are essential. This includes routine assessments of blood glucose levels, blood pressure, and cholesterol, as well as kidney function tests.
- Medication Adherence: Taking prescribed medications consistently, whether for diabetes, blood pressure, or cholesterol, is crucial in maintaining optimal systemic factors that can influence DR.
- Lifestyle Modifications: Adopting a healthy lifestyle, which includes a balanced diet, regular exercise, and stress management, can positively impact systemic factors and contribute to better control of diabetes and its complications.
- Weight Management: Achieving and maintaining a healthy weight can improve insulin sensitivity and glycemic control, which are key factors in preventing and managing DR.
By addressing these systemic factors, individuals with diabetes can significantly reduce their risk of developing or progressing diabetic retinopathy. It’s important to work closely with healthcare providers, including ophthalmologists and primary care physicians, to develop a comprehensive treatment plan that addresses both the systemic and ocular aspects of diabetes management. Regular monitoring and adherence to prescribed treatments are essential for maintaining optimal eye health in individuals with diabetes.
Treatment for NPDR may involve closely managing diabetes and, in some cases, laser therapy to help prevent further damage to the retina. It’s important to work closely with a healthcare professional, such as an ophthalmologist or an optometrist, to develop a personalized treatment plan and to receive regular eye check-ups to monitor the condition. Early intervention and proper management can significantly reduce the risk of vision loss associated with NPDR.
Treatment options for DME can include laser therapy to reduce swelling, injections of medications into the eye, or in some cases, surgery.
Intravitreal injections are one of the available treatments for diabetic macular edema (DME). These injections involve the delivery of medication directly into the vitreous, the gel-like substance inside the eye. The medication helps reduce swelling and inflammation in the macula, which is the central part of the retina responsible for sharp, central vision.
There are several types of medications that can be administered via intravitreal injection for DME:
- Anti-VEGF (Vascular Endothelial Growth Factor) Agents: These drugs work by inhibiting the growth of abnormal blood vessels and reducing leakage from existing vessels. Some commonly used anti-VEGF agents for DME include:
- Ranibizumab (Lucentis)
- Bevacizumab (Avastin)
- Aflibercept (Eylea)
- Corticosteroids: Steroids can help reduce inflammation and swelling in the retina. Intravitreal corticosteroid injections may be used for cases of DME that do not respond well to anti-VEGF treatment. Common corticosteroid options include:
- Dexamethasone implant (Ozurdex)
- Fluocinolone acetonide implant (Iluvien)
The choice of medication and the frequency of injections will be determined by your ophthalmologist based on factors such as the severity of DME, your response to previous treatments, and any other underlying eye conditions.
It’s important to note that while intravitreal injections can be highly effective in reducing macular edema and improving vision in many cases, they may require regular follow-up injections to maintain their benefits. The treatment plan will be tailored to your specific needs and monitored closely by your healthcare provider.
As with any medical procedure, there are potential risks and benefits associated with intravitreal injections. Your ophthalmologist will discuss these with you and provide detailed information to help you make an informed decision about your treatment. If you have been diagnosed with DME or have concerns about your eye health, it’s essential to consult with your healthcare provider for personalized advice and recommendations.Top of Form
Treatment for PDR may involve laser surgery to seal leaking blood vessels and shrink abnormal ones, or injections of medications directly into the eye to help stabilize the condition. In more severe cases, vitrectomy surgery may be necessary to remove blood and scar tissue from the eye.
.
